Okay, so here’s the deal. I recently had to dive into the world of healthcare appeals, specifically with Molina Healthcare. It all started when I received a denial letter from Molina for a medical service I thought should have been covered. I was surprised and frankly, a bit lost. I knew I had to appeal, but I had no idea where to start.
First things first, I had to figure out the deadline. Turns out, I had 90 calendar days from the date on Molina’s denial letter to get my appeal in. Phew, at least I had some time. I decided to gather all the information I could about my case. I had the option to present my case in person or in writing. I opted for writing, thinking it would be easier to organize my thoughts and the necessary documents.
Next, I needed to find the right form. After some digging, I discovered that Molina has a specific form for this, called the “Provider Appeal/Dispute Form,” which I found on their website. I also learned that I could get help with filing the appeal. They had a number to call (800-869-7165) if you need help, which I thought was pretty considerate. You can also appoint someone to represent you, like a lawyer or even a provider. You just have to sign a consent form to let them represent you.
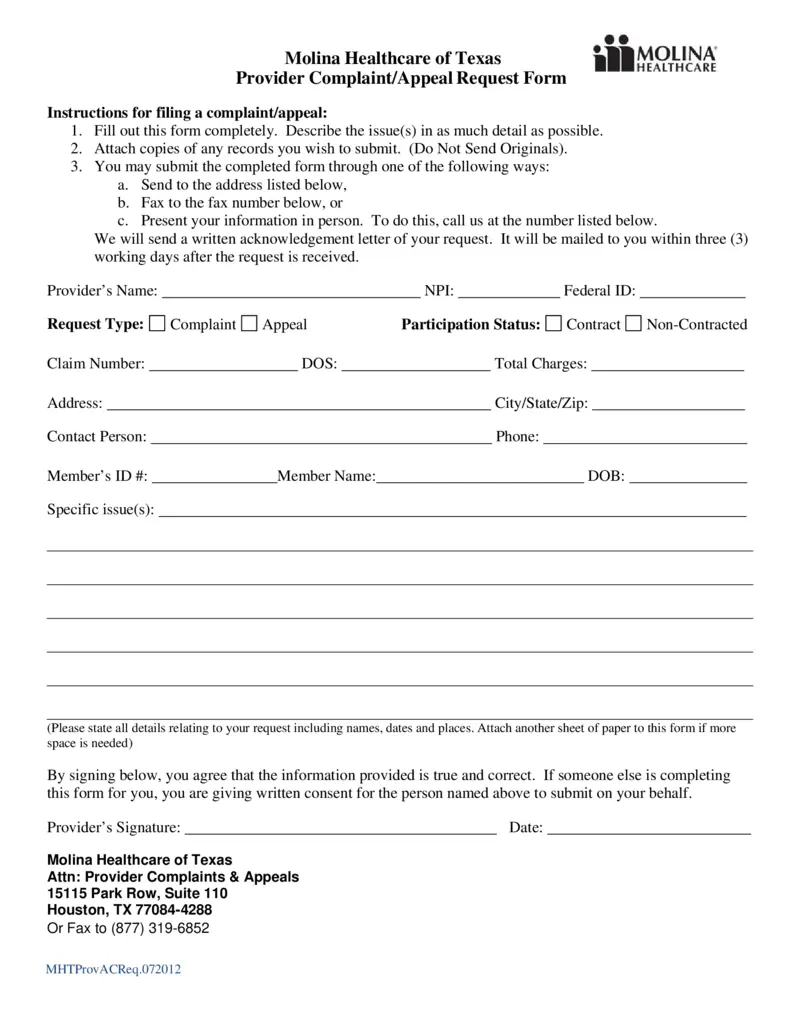
I decided to handle it myself for now. I started by carefully reading the instructions on the form. It mentioned something called an “Authorization Appeal,” which is basically an appeal for a prior authorization denial. I made sure to fill out every section of the form accurately, providing as much detail as possible about the service that was denied and why I believed it should be covered.
Once the form was filled out, I double-checked everything and gathered supporting documents, like medical records and notes from my doctor. I wanted to make my case as strong as possible. After that I mailed the completed form along with the supporting documents to the address they gave.
After sending in the appeal, I waited. It felt like forever, but eventually, I received a written acknowledgment from Molina Healthcare. I found out that for providers, Molina Healthcare of Idaho allows 60 days from the date of denial to file an appeal, and they can submit it through the Availity Essentials Provider Portal. While I was waiting, I also made some calls to their member services to follow up and make sure they had everything they needed.
Finally, I got the decision. It wasn’t what I had hoped for, but at least I knew I had done everything I could. The whole process was a bit of a headache, but I learned a lot about how to navigate the healthcare appeal system. It’s definitely not something I want to go through again, but if I have to, I’ll be much better prepared next time.